

The RCA should focus on vulnerabilities in systems and processes, not on the individual(s).
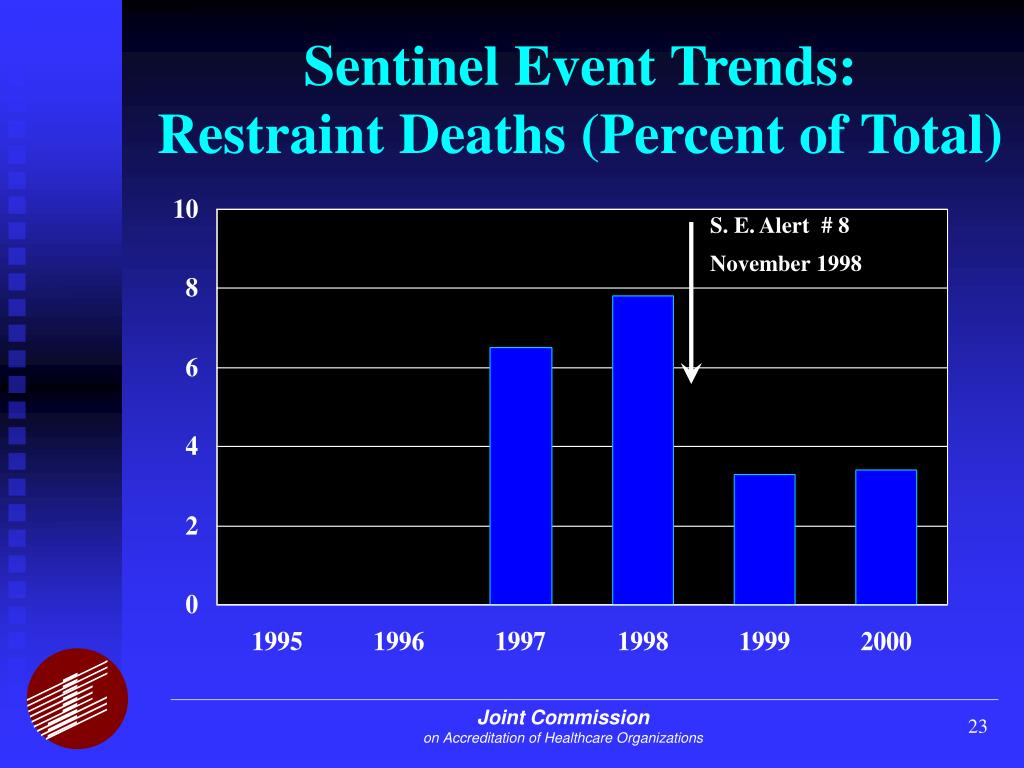
Joint commission falls sentinel event series#
The RCA involves repeatedly asking a series of “why” questions until the root systemic causal factor(s) that culminated in the sentinel event is identified. The hospital can utilize this template, consisting of multiple analysis questions and prompts, or utilize a similar framework for identifying the causal factors.

The Joint Commission provides a framework for the RCA. The steps in an RCA include identifying the team, information gathering, organizing information, identifying contributing factors, and drilling down to the root cause. The process should commence within 72 hours of the event. The reporting organization should prepare and submit a thorough root cause analysis and action plan within 45 days of the sentinel event. Required Response to a Reviewable Sentinel Event Hemolytic transfusion reactions due to major blood group incompatibilities are still reported with an incidence of 7-9 per year.Īn appropriate response to a sentinel event may include the following: Fortunately, infant discharge to the wrong family has been reduced to zero. The risk of suicide is the highest immediately following hospitalization, during the inpatient stay, or immediately post-discharge. They are followed by suicide, delay in treatment, and medication errors. The most common sentinel events are wrong-site surgery, foreign body retention, and falls. More than three-fourths of them are voluntarily reported to the agency. The great majority occur in a medical/surgical hospital setting, followed by psychiatric hospitals (including psychiatric units and clinics) and emergency departments. Sentinel events occur in every healthcare setting. Since 2007, about 800 sentinel events are reported to the Joint Commission every year according to their summary data of sentinel events. All accredited hospitals are encouraged but not obligated to report to the Joint Commission every sentinel event. Reporting of sentinel events to The Joint Commission is a voluntary process, and no conclusions should be drawn about the actual relative frequency of events or trends in events over time.The hospital must review all sentinel events. The remaining sentinel events were reported either by patients or their families, or employees of a healthcare organization. Most sentinel events (90%) were voluntarily self-reported to The Joint Commission by an accredited or certified healthcare organization. Of all the sentinel events, 20% were associated with patient death, 44% with severe temporary harm and 13% with unexpected additional care/extended stay. Most reported sentinel events occurred in a hospital (88%).

Unintended retention of foreign object (6%)įailures in communications, teamwork and consistently following polices were the leading causes for reported sentinel events.The most prevalent sentinel event types were: The Joint Commission reviewed 1,441 sentinel events in 2022. Sentinel events are debilitating to both patients and healthcare providers involved in the event. A sentinel event is a patient safety event that results in death, permanent harm or severe temporary harm. The Joint Commission has released its Sentinel Event Data 2022 Annual Review on serious adverse events from Jan.


 0 kommentar(er)
0 kommentar(er)
